Get your Free Calisthenics Certification
100% Online Training — Study Wherever You Are
What You'll Get
Discover what makes our approach unique
Online quizzes
Online quizzes to practice your knowledge
Flexible learning
Live or self-paced learning
Open to everyone
No prior knowledge or degree required
Popular Articles
Our most popular articles to get you started

How to Fix Tight Hip Flexors: Best Stretches, Exercises & Daily Routine
Complete guide to relieving tight hip flexors with evidence-based stretches, strengthening exercises, and a daily routine. Learn causes, symptoms, self-tests, and how tight hips affect your calisthenics training.

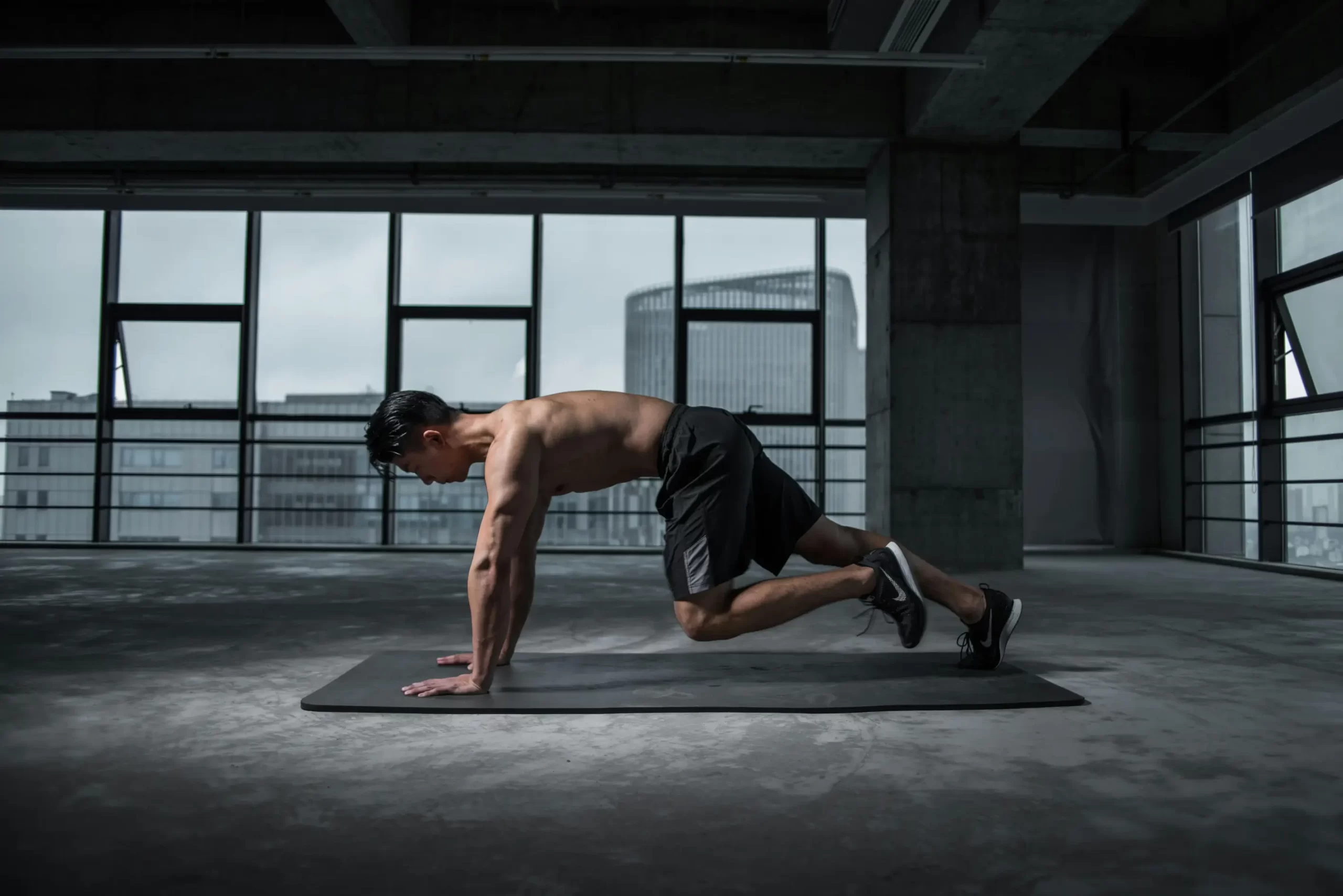
Calisthenics for Beginners: Complete 30-Day Program
Start your calisthenics journey with this free 30-day beginner workout plan. Build strength, improve mobility, and master fundamental bodyweight exercises with step-by-step progressions.

How to Fix Anterior Pelvic Tilt: Evidence-Based Exercises, Stretches & Posture Correction
Complete guide to correcting anterior pelvic tilt with proven exercises, stretches, and lifestyle modifications. Learn the anatomy, causes, and step-by-step rehabilitation protocol.
Featured Courses
Professional certification programs to advance your career
Popular Lessons
Start learning with our most popular content
What You'll Learn
Complete curriculum covering everything from anatomy to advanced programming
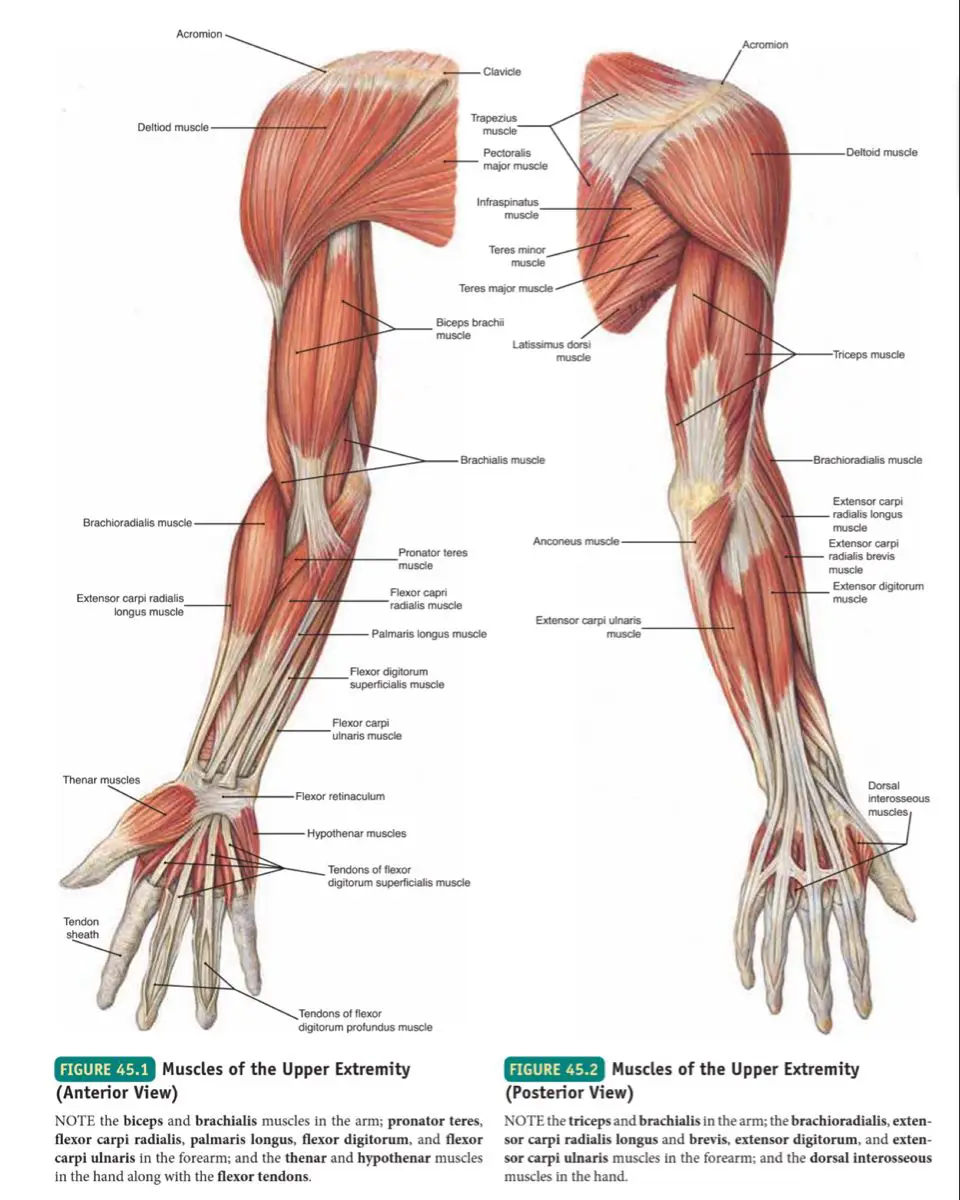
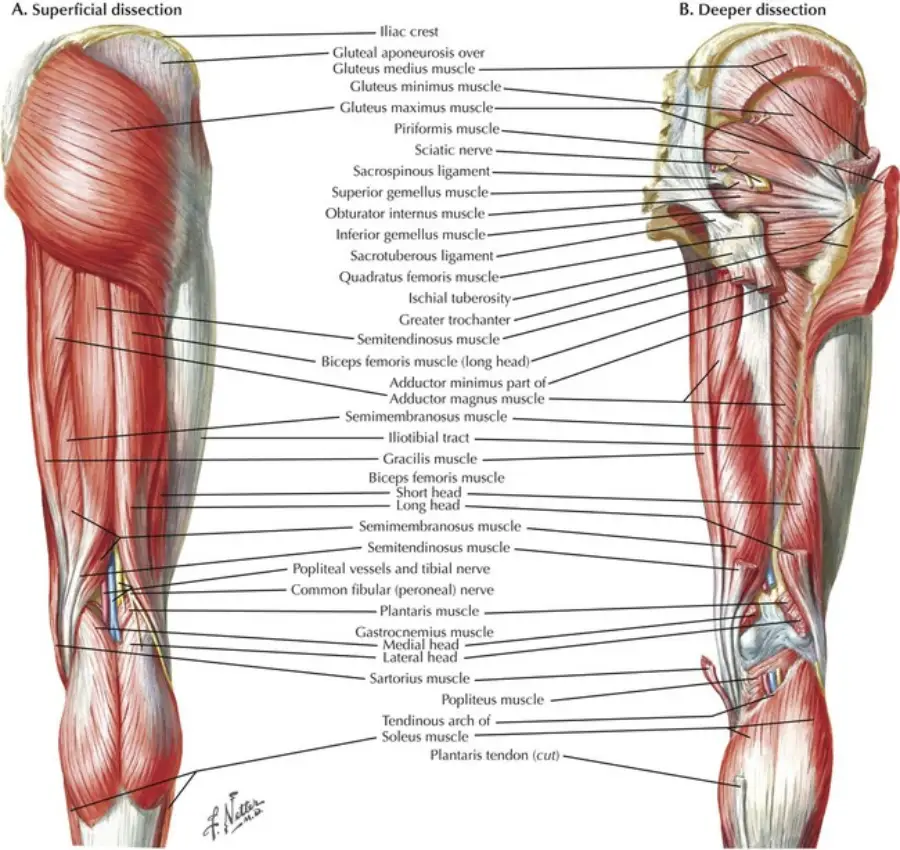
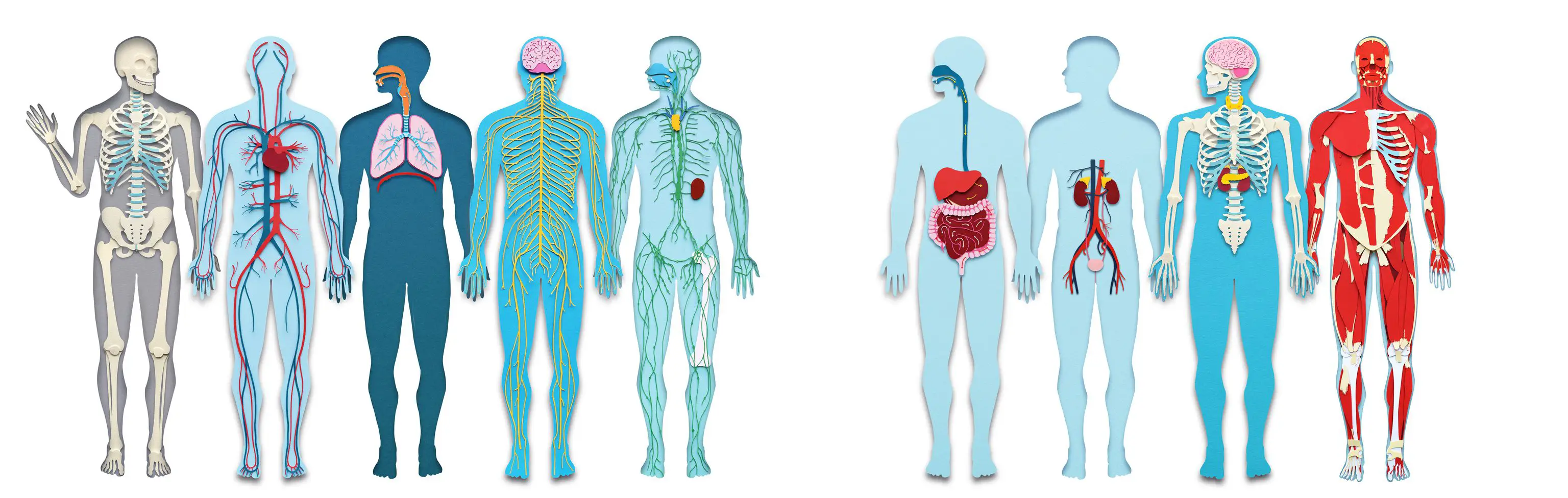
Anatomy & Kinesiology
- Musculoskeletal system fundamentals
- Biomechanics and movement patterns
- Injury prevention and rehabilitation
Training Methodology
- Progressive overload principles
- Program design and periodization
- Exercise progressions and regressions
Exercise Science
- Muscle physiology and adaptation
- Energy systems and metabolism
- Recovery and nutrition basics
Professional Skills
- Client assessment techniques
- Coaching and communication
- Safety and risk management
Latest Articles
Evidence-based fitness insights

Hip Impingement in Squats: How to Train Pain-Free
Learn what hip impingement (FAI) is, how it affects squatting, signs and symptoms, squat modifications, mobility exercises, and when to seek professional help.
Read More
Thoracic Spine Mobility: How to Fix Upper Back Stiffness
Complete guide to improving thoracic spine mobility and fixing upper back stiffness. Learn assessment tests, the best thoracic mobility exercises, and how t-spine mobility affects calisthenics performance.
Read More
Flat Back Posture: Causes, Symptoms & Corrective Exercises for Lumbar Lordosis Loss
Learn what causes flat back posture (loss of lumbar lordosis), how to identify it, and evidence-based corrective exercises and mobility work to restore your natural spinal curve.
Read MoreFrequently Asked Questions
About Calisthenics Association
Unlock your potential with the first online school offering FREE Calisthenics training certification! Our comprehensive, fully online courses allow you to become a certified Calisthenics trainer from anywhere in the world. Join thousands of students across the globe who have transformed their lives and careers with our expert training. Why wait? Start your journey with us today and embrace the future of fitness training. The world of Calisthenics awaits you!