Male Genital Organs: Structure, Function, and Clinical Relevance
Abstract
The male genital organs are essential for reproduction, sexual function, and the production of male sex hormones. These organs are divided into internal and external structures, each playing a specific role in spermatogenesis, sperm transport, and hormonal regulation. This article provides an in-depth overview of the anatomy, function, and clinical significance of the male genital organs, highlighting their roles in reproduction and overall male health.
Introduction
The male reproductive system is designed for the production, maturation, and delivery of sperm, as well as the secretion of male sex hormones, primarily testosterone. The male genital organs include both external and internal components. The external organs are involved in sexual intercourse and sperm ejaculation, while the internal organs are responsible for sperm production, maturation, and transportation. The male reproductive system interacts closely with the endocrine system to regulate reproductive function.
Anatomy of the Male Genital Organs
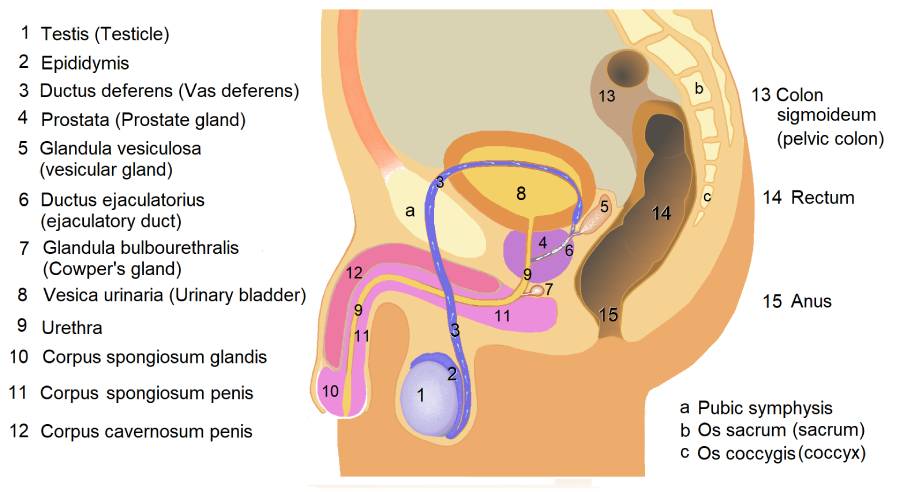
The male genital organs are categorized into external and internal structures:
- External Genital Organs
- Internal Genital Organs
External Genital Organs
The external genitalia of the male reproductive system consist of the penis and scrotum.
- Penis
-
Location: The penis is located externally at the front of the pelvis.
-
Structure: The penis is composed of three cylindrical columns of erectile tissue surrounded by skin. These columns include:
- Corpora Cavernosa: Two larger columns of erectile tissue located dorsally.
- Corpus Spongiosum: A single column of erectile tissue that surrounds the urethra and forms the glans penis, the rounded tip of the penis.
The penis also contains the urethra, which serves as a common pathway for the excretion of urine and the ejaculation of semen.
-
Function: The penis is responsible for delivering sperm into the female reproductive tract during sexual intercourse. During arousal, the corpora cavernosa and corpus spongiosum become engorged with blood, leading to an erection. The glans penis contains numerous nerve endings, contributing to sexual sensation.
-
Clinical Relevance: Conditions affecting the penis include erectile dysfunction (inability to maintain an erection), Peyronie’s disease (fibrous scar tissue causing penile curvature), and penile cancer.
-
- Scrotum
- Location: The scrotum is a sac of skin located below the penis, containing the testes.
- Structure: The scrotum is divided into two compartments, each housing one testis, epididymis, and part of the spermatic cord. The scrotum is lined with smooth muscle (the dartos muscle), which helps regulate the temperature of the testes by contracting or relaxing to move the testes closer to or away from the body.
- Function: The scrotum protects the testes and helps maintain a temperature about 2-3°C below body temperature, which is essential for normal sperm production.
- Clinical Relevance: Scrotal conditions include varicocele (enlargement of veins in the scrotum), hydrocele (fluid accumulation around the testicles), and testicular torsion, a medical emergency in which the spermatic cord becomes twisted, cutting off blood supply to the testicle.
Internal Genital Organs
The internal male genital organs include the testes, epididymis, vas deferens, seminal vesicles, prostate gland, and bulbourethral glands.
- Testes (Testicles)
- Location: The testes are paired, oval-shaped glands located within the scrotum.
- Structure: Each testis is divided into lobules that contain seminiferous tubules, where sperm production (spermatogenesis) takes place. The Leydig cells, located between the seminiferous tubules, produce testosterone.
- Function: The testes have two primary functions:
- Spermatogenesis: The production of sperm, which begins at puberty and continues throughout life.
- Hormone Production: The Leydig cells produce testosterone, the primary male sex hormone responsible for the development of male secondary sexual characteristics (such as increased muscle mass, body hair, and a deeper voice) and the regulation of libido and spermatogenesis.
- Clinical Relevance: Testicular conditions include testicular cancer, cryptorchidism (undescended testicles), and orchitis (inflammation of the testicles, often due to infection).
- Epididymis
- Location: The epididymis is a coiled tube located on the posterior surface of each testis.
- Structure: The epididymis is divided into three regions: the head, body, and tail. It is continuous with the vas deferens.
- Function: The epididymis is responsible for the maturation and storage of sperm. Sperm cells gain the ability to move and fertilize an egg as they pass through the epididymis.
- Clinical Relevance: Infections of the epididymis, known as epididymitis, can cause pain and swelling in the scrotum. It is often caused by sexually transmitted infections (STIs) or urinary tract infections.
- Vas Deferens (Ductus Deferens)
- Location: The vas deferens is a muscular tube that extends from the epididymis to the ejaculatory ducts.
- Structure: It is a thick-walled tube that travels within the spermatic cord, passes through the inguinal canal, and enters the pelvic cavity before joining the seminal vesicle to form the ejaculatory duct.
- Function: The vas deferens transports mature sperm from the epididymis to the ejaculatory duct in preparation for ejaculation.
- Clinical Relevance: Vasectomy is a common surgical procedure for male sterilization in which the vas deferens is cut and sealed to prevent the transport of sperm.
- Seminal Vesicles
- Location: The seminal vesicles are paired glands located posterior to the bladder and lateral to the vas deferens.
- Structure: Each seminal vesicle is about 5 cm long and has a highly folded structure.
- Function: The seminal vesicles secrete a thick, alkaline fluid that makes up about 60-70% of semen. This fluid contains fructose, which provides energy for the sperm, and prostaglandins, which promote sperm motility and viability.
- Clinical Relevance: Infections or inflammation of the seminal vesicles can lead to vesiculitis, which may cause pain and affect semen quality.
- Prostate Gland
- Location: The prostate is a walnut-sized gland located just below the bladder, surrounding the upper part of the urethra.
- Structure: The prostate consists of glandular tissue and smooth muscle fibers, with ducts that empty into the prostatic urethra.
- Function: The prostate secretes a milky fluid that makes up about 30% of semen. This fluid is slightly acidic and contains enzymes, such as prostate-specific antigen (PSA), which help liquefy semen after ejaculation, allowing sperm to swim freely.
- Clinical Relevance: Common prostate conditions include benign prostatic hyperplasia (BPH), a non-cancerous enlargement of the prostate that can obstruct urine flow, and prostate cancer, one of the most common cancers in men. PSA testing is often used to screen for prostate cancer.
- Bulbourethral Glands (Cowper’s Glands)
- Location: The bulbourethral glands are two small glands located below the prostate, near the base of the penis.
- Structure: Each gland is about the size of a pea and connects to the urethra via a small duct.
- Function: These glands secrete a clear, mucus-like fluid during sexual arousal. This fluid lubricates the urethra and neutralizes any residual acidity from urine, preparing the urethra for the passage of semen.
- Clinical Relevance: Disorders of the bulbourethral glands are rare but can include blockages or inflammation, known as Cowper’s duct obstruction.
Spermatogenesis
Spermatogenesis is the process by which sperm cells are produced in the seminiferous tubules of the testes. It involves several stages:
- Spermatogonia: These are the diploid stem cells located in the seminiferous tubules that divide by mitosis to form primary spermatocytes.
- Primary Spermatocytes: These cells undergo meiosis I to produce two haploid secondary spermatocytes.
- Secondary Spermatocytes: These undergo meiosis II to produce four haploid spermatids.
- Spermatids: These immature sperm cells undergo a process called spermiogenesis, during which they develop a flagellum (tail), condense their DNA, and form a compact head. They then enter the epididymis for further maturation.
Spermatogenesis is regulated by hormones, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), and testosterone, which is produced by the Leydig cells in response to LH.
Ejaculation and Semen
Ejaculation is the process by which semen, a mixture of sperm and glandular fluids, is expelled from the body through the urethra during orgasm. The process occurs in two phases:
- Emission: Semen is moved into the urethra from the vas deferens and accessory glands.
- Ejaculation: Rhythmic contractions of the pelvic muscles, along with smooth muscle in the vas deferens and accessory glands, propel semen out of the body.
Semen is composed of:
- Sperm cells from the testes
- Fluids from the seminal vesicles, which provide energy and support for sperm
- Prostate fluid, which helps sperm mobility
- Mucus from the bulbourethral glands, which lubricates the urethra
Clinical Relevance
Several conditions can affect the male genital organs, leading to reproductive, urinary, or sexual dysfunction:
- Erectile Dysfunction (ED): Inability to achieve or maintain an erection sufficient for sexual intercourse. ED can be caused by vascular, neurological, or psychological factors, and treatments include medications like phosphodiesterase inhibitors (e.g., Viagra), lifestyle changes, and surgery.
- Testicular Cancer: A rare but highly treatable cancer that typically affects younger men. Symptoms may include a lump or swelling in the testicle. Early detection through self-examination and ultrasound is crucial for successful treatment.
- Prostate Disorders: Benign prostatic hyperplasia (BPH) causes urinary symptoms such as difficulty starting urination, weak urine flow, and frequent urination. Prostate cancer, in contrast, may be asymptomatic in its early stages but can spread to other parts of the body if not treated early.
- Infertility: Male infertility may be caused by low sperm count, poor sperm motility, or blockages in the reproductive tract. Treatment options range from medication to assisted reproductive technologies, such as in vitro fertilization (IVF).
Conclusion
The male genital organs play essential roles in reproduction, sexual function, and hormone production. Understanding their anatomy and function is critical for diagnosing and managing conditions that affect male reproductive health. Advances in medical treatments and reproductive technologies have greatly improved the outcomes for men facing reproductive health issues, enhancing both fertility and overall well-being.
References
- Standring, S. (2020). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (42nd ed.). Elsevier.
- Moore, K. L., Dalley, A. F., & Agur, A. M. R. (2013). Clinically Oriented Anatomy (7th ed.). Lippincott Williams & Wilkins.
- Wein, A. J., & Kavoussi, L. R. (2016). Campbell-Walsh Urology (11th ed.). Elsevier.
- McAninch, J. W., & Lue, T. F. (2013). Smith & Tanagho’s General Urology (18th ed.). McGraw-Hill.
- American Urological Association. Guidelines on Prostate Cancer and Erectile Dysfunction.
This detailed exploration of the male genital organs highlights their importance in reproductive and sexual health, emphasizing the need for early diagnosis and treatment of associated conditions.
🎓 Want to become a certified instructor?
This lesson is part of our FREE Anatomy course. Create a free account to track your progress and earn your certificate!