The Peripheral Nervous System: Structure, Function, and Clinical Relevance
Abstract
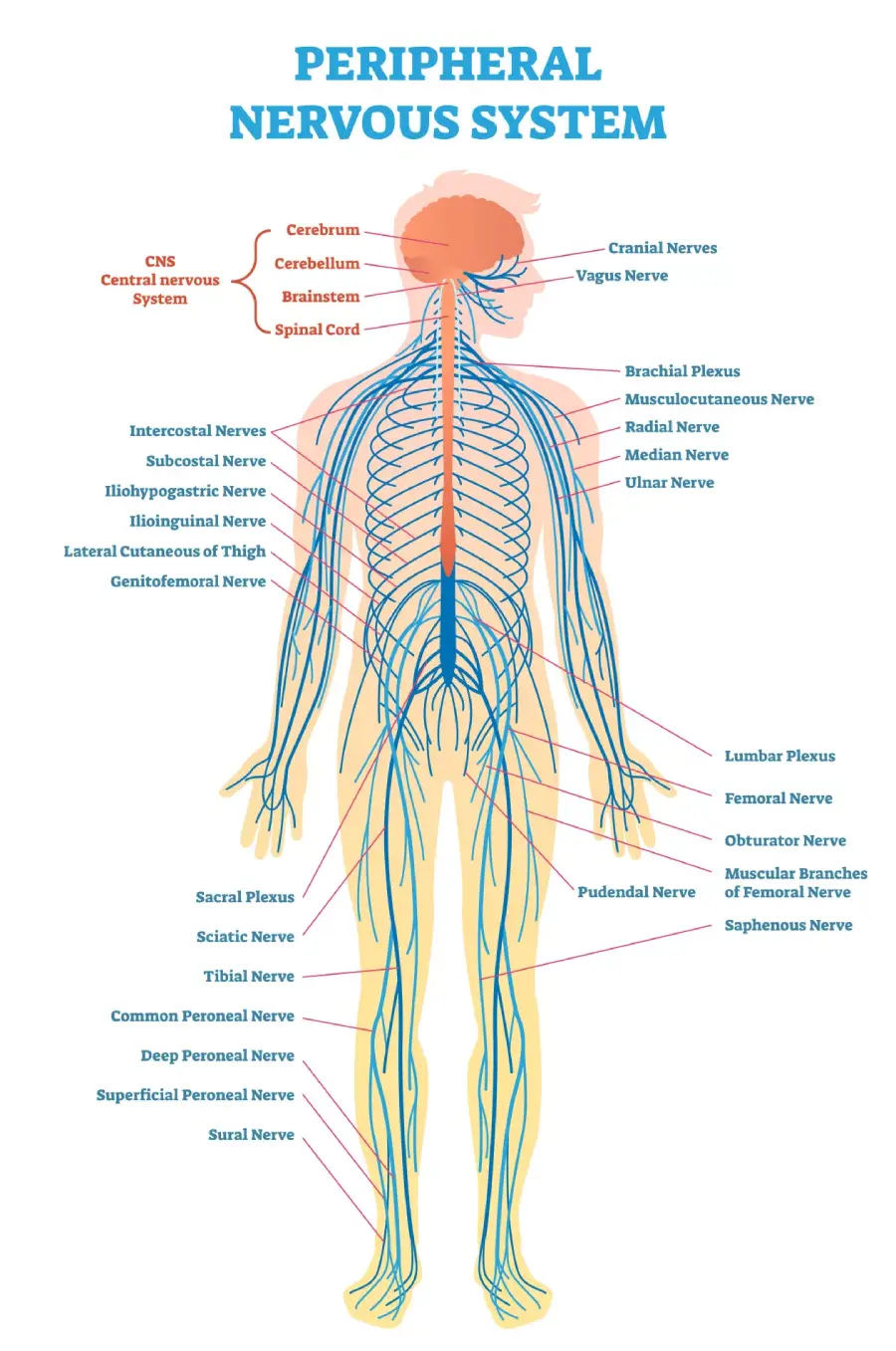
The peripheral nervous system (PNS) plays a critical role in connecting the central nervous system (CNS) to the rest of the body. It comprises the nerves and ganglia outside the brain and spinal cord and is responsible for transmitting sensory and motor information between the CNS and the limbs, organs, and tissues. The PNS is divided into the somatic and autonomic nervous systems, each with distinct functions. This article provides a comprehensive examination of the anatomy, functions, and clinical significance of the peripheral nervous system.
Introduction
The peripheral nervous system is an essential component of the nervous system, allowing communication between the CNS and the body’s various regions. It consists of nerves that transmit sensory inputs from the body to the CNS (afferent pathways) and motor commands from the CNS to the body (efferent pathways). The PNS includes cranial nerves, spinal nerves, and autonomic nerves, which control involuntary functions such as heart rate, digestion, and glandular activity.
Structure of the Peripheral Nervous System
The PNS consists of a vast network of nerves that branch from the CNS and extend throughout the body. These nerves are divided into two main types:
- Cranial Nerves
- Spinal Nerves
Additionally, the PNS is functionally divided into two major subdivisions:
- Somatic Nervous System (SNS)
- Autonomic Nervous System (ANS)
Cranial Nerves
The cranial nerves are 12 pairs of nerves that emerge directly from the brain and brainstem, each with specific sensory, motor, or mixed functions.
- Olfactory Nerve (I): Transmits sensory information related to smell.
- Optic Nerve (II): Transmits visual information from the retina to the brain.
- Oculomotor Nerve (III): Controls most of the eye’s movements, pupil constriction, and lens accommodation.
- Trochlear Nerve (IV): Controls the superior oblique muscle, which moves the eye downward and laterally.
- Trigeminal Nerve (V): Provides sensory input from the face and controls muscles for mastication.
- Abducens Nerve (VI): Controls the lateral rectus muscle, which abducts the eye.
- Facial Nerve (VII): Controls muscles of facial expression, taste sensation from the anterior two-thirds of the tongue, and secretions from the lacrimal and salivary glands.
- Vestibulocochlear Nerve (VIII): Transmits sensory information for hearing and balance.
- Glossopharyngeal Nerve (IX): Provides taste sensation from the posterior one-third of the tongue and innervates muscles involved in swallowing.
- Vagus Nerve (X): Controls autonomic functions of the heart, lungs, and digestive tract and provides sensation from the throat, larynx, and abdominal organs.
- Accessory Nerve (XI): Controls the sternocleidomastoid and trapezius muscles involved in head and shoulder movements.
- Hypoglossal Nerve (XII): Controls movements of the tongue.
Spinal Nerves
The spinal nerves are 31 pairs of mixed nerves that emerge from the spinal cord and innervate different regions of the body. Each spinal nerve has both sensory (afferent) and motor (efferent) fibers.
- Cervical Nerves (C1-C8): Innervate the neck, diaphragm, and upper limbs.
- Thoracic Nerves (T1-T12): Innervate the thoracic region, including the chest and abdominal muscles.
- Lumbar Nerves (L1-L5): Innervate the lower back, hips, and parts of the legs.
- Sacral Nerves (S1-S5): Innervate the pelvic region, bladder, and lower limbs.
- Coccygeal Nerve (Co1): A small nerve innervating the tailbone area.
Each spinal nerve branches into a dorsal ramus (supplying the back muscles and skin) and a ventral ramus (supplying the limbs and anterior body wall). The spinal nerves also form networks called plexuses:
- Cervical Plexus: Supplies the neck and diaphragm.
- Brachial Plexus: Innervates the shoulder, arm, forearm, and hand.
- Lumbar Plexus: Innervates the lower abdomen, thigh, and part of the leg.
- Sacral Plexus: Innervates the pelvis, buttocks, and lower limb, including the sciatic nerve, the largest nerve in the body.
Functional Subdivisions of the Peripheral Nervous System
The PNS is functionally divided into two main parts: the somatic nervous system and the autonomic nervous system.
Somatic Nervous System (SNS)
The somatic nervous system controls voluntary movements and transmits sensory information to the CNS. It is responsible for conscious perception and motor control of skeletal muscles.
- Afferent Pathways: Sensory neurons in the SNS carry information from the skin, muscles, and joints to the CNS. These sensory inputs include touch, pain, temperature, and proprioception (sense of body position).
- Efferent Pathways: Motor neurons in the SNS send signals from the CNS to skeletal muscles, allowing voluntary movement.
Autonomic Nervous System (ANS)
The autonomic nervous system regulates involuntary physiological functions, such as heart rate, digestion, and respiration. It is divided into two branches:
- Sympathetic Nervous System: Prepares the body for "fight or flight" responses during stress or emergencies. It increases heart rate, dilates pupils, relaxes the bronchi, and diverts blood flow to skeletal muscles.
- Parasympathetic Nervous System: Controls "rest and digest" functions, conserving energy and promoting homeostasis. It slows the heart rate, constricts the bronchi, stimulates digestion, and promotes glandular activity.
The enteric nervous system (ENS) is often considered part of the ANS and is responsible for regulating gastrointestinal function independently of the CNS.
Function of the Peripheral Nervous System
The PNS plays several critical roles in the body:
- Sensory Function: The PNS transmits sensory information from receptors in the skin, muscles, and organs to the CNS. This includes sensations such as pain, temperature, touch, and proprioception.
- Motor Function: The PNS carries motor signals from the CNS to skeletal muscles, allowing voluntary movements such as walking, lifting, and speaking.
- Autonomic Control: The ANS component of the PNS regulates involuntary functions, such as blood pressure, heart rate, respiration, digestion, and glandular secretion.
- Homeostasis: By balancing the sympathetic and parasympathetic branches, the PNS helps maintain homeostasis by adjusting physiological functions in response to internal and external changes.
Clinical Relevance
Disorders affecting the PNS can lead to a variety of clinical problems, often impacting motor function, sensation, and autonomic control.
- Peripheral Neuropathy: Damage to the peripheral nerves can result in weakness, numbness, and pain, commonly affecting the hands and feet. Causes include diabetes, autoimmune diseases, infections, and toxins.
- Carpal Tunnel Syndrome: Compression of the median nerve at the wrist can lead to pain, numbness, and weakness in the hand.
- Sciatica: Compression or irritation of the sciatic nerve causes radiating pain, numbness, or tingling down the leg.
- Bell’s Palsy: A form of facial paralysis caused by damage or inflammation of the facial nerve (cranial nerve VII), leading to weakness or drooping of the facial muscles.
- Guillain-Barré Syndrome: An autoimmune disorder that affects the peripheral nerves, leading to rapid onset of muscle weakness and paralysis. It often begins in the lower limbs and can spread to the upper body and respiratory muscles.
- Diabetic Neuropathy: A common complication of diabetes, causing damage to peripheral nerves, particularly in the legs and feet, leading to pain, numbness, and a loss of sensation.
- Autonomic Neuropathy: Affects the autonomic nerves and can result in abnormalities in heart rate, blood pressure, digestion, and bladder function.
Diagnostic and Therapeutic Approaches
The diagnosis of PNS disorders typically involves clinical examination, imaging studies, and functional tests.
- Electromyography (EMG): A diagnostic tool that measures the electrical activity of muscles to detect abnormalities in nerve function.
- Nerve Conduction Studies: Used to assess the speed and strength of electrical signals traveling through peripheral nerves.
- MRI and CT Scans: Imaging studies that help visualize structural abnormalities in nerves and surrounding tissues.
- Blood Tests: Useful for identifying underlying conditions like diabetes or autoimmune disorders that can contribute to peripheral nerve damage.
- Medications: Pain relievers, anticonvulsants, and antidepressants are often prescribed to manage the pain associated with peripheral neuropathy.
- Physical Therapy: Exercises and rehabilitation can help maintain muscle strength and mobility in patients with motor nerve damage.
- Surgery: In cases of nerve compression, such as carpal tunnel syndrome, surgical intervention may be required to relieve pressure on the affected nerve.
Conclusion
The peripheral nervous system is vital for communication between the CNS and the body, regulating voluntary and involuntary functions. Understanding the anatomy and functions of the PNS is crucial for diagnosing and managing peripheral nerve disorders. Advances in diagnostic techniques and treatment options continue to improve outcomes for individuals with peripheral nervous system diseases, enhancing their quality of life.
References
- Standring, S. (2020). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (42nd ed.). Elsevier.
- Kandel, E. R., Schwartz, J. H., & Jessell, T. M. (2012). Principles of Neural Science (5th ed.). McGraw-Hill.
- Moore, K. L., Dalley, A. F., & Agur, A. M. R. (2013). Clinically Oriented Anatomy (7th ed.). Lippincott Williams & Wilkins.
- Netter, F. H. (2014). Atlas of Human Anatomy (6th ed.). Elsevier.
- Said, G. (2007). Diabetic neuropathy—a review. Nature Clinical Practice Neurology, 3(6), 331-340.
- Dyck, P. J., & Thomas, P. K. (2005). Peripheral Neuropathy (4th ed.). Elsevier.
This comprehensive exploration of the peripheral nervous system highlights its importance in maintaining bodily functions and underscores the need for ongoing research in the diagnosis and treatment of PNS disorders.
🎓 Want to become a certified instructor?
This lesson is part of our FREE Anatomy course. Create a free account to track your progress and earn your certificate!