The Urinary System: Structure, Function, and Clinical Relevance
Abstract
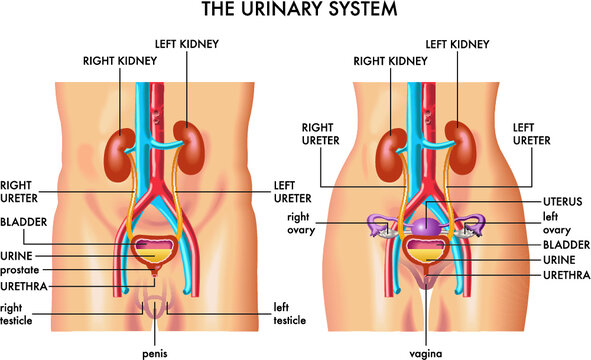
The urinary system, also known as the renal system, is responsible for filtering waste products from the blood, regulating fluid and electrolyte balance, and maintaining homeostasis in the body. It consists of the kidneys, ureters, bladder, and urethra, which work together to produce, store, and eliminate urine. This article provides a comprehensive overview of the anatomy, function, and clinical significance of the urinary system.
Introduction
The urinary system plays a vital role in maintaining the body’s internal environment by regulating the composition of blood, eliminating metabolic waste products, and controlling water and electrolyte balance. It also helps maintain blood pressure and contributes to red blood cell production. Understanding the urinary system’s anatomy and physiology is crucial for diagnosing and managing renal diseases and disorders.
Anatomy of the Urinary System
The urinary system is composed of four main organs:
- Kidneys
- Ureters
- Urinary Bladder
- Urethra
1. Kidneys
- Location: The kidneys are paired, bean-shaped organs located retroperitoneally on either side of the spine, just below the rib cage. The right kidney is slightly lower than the left due to the position of the liver.
- Structure: Each kidney is about 10-12 cm long and consists of three main regions:
- Cortex: The outer region where filtration occurs.
- Medulla: Contains renal pyramids, which funnel urine into the renal pelvis.
- Renal Pelvis: A funnel-shaped structure that collects urine and channels it into the ureter.The kidneys are highly vascular, receiving approximately 20-25% of the cardiac output through the renal arteries. Blood enters the kidneys for filtration and exits through the renal veins.
- Nephrons: The functional units of the kidneys, nephrons are microscopic structures that filter blood and form urine. Each kidney contains around one million nephrons, which are composed of:
- Glomerulus: A network of capillaries where blood filtration begins.
- Bowman’s Capsule: A structure that encases the glomerulus and collects the filtrate.
- Proximal Convoluted Tubule (PCT): The site of nutrient and water reabsorption.
- Loop of Henle: A long loop that concentrates urine and reabsorbs water.
- Distal Convoluted Tubule (DCT): Fine-tunes ion balance and pH regulation.
- Collecting Duct: Collects urine from multiple nephrons and transports it to the renal pelvis.
2. Ureters
- Location: The ureters are muscular tubes that extend from the renal pelvis to the urinary bladder.
- Structure: Each ureter is about 25-30 cm long and is lined with smooth muscle that contracts rhythmically (peristalsis) to propel urine from the kidneys to the bladder.
- Function: The ureters transport urine from the kidneys to the urinary bladder.
3. Urinary Bladder
- Location: The bladder is a hollow, muscular organ located in the pelvis, just behind the pubic bone.
- Structure: The bladder is lined with transitional epithelium and can expand significantly as it fills with urine. It has a muscular layer called the detrusor muscle, which contracts during urination.
- Function: The bladder stores urine until it is excreted from the body. It can hold approximately 400-600 mL of urine in adults. The bladder has two sphincters:
- Internal Urethral Sphincter: Involuntary control; located at the bladder neck.
- External Urethral Sphincter: Voluntary control; located in the pelvic floor muscles.
4. Urethra
- Location: The urethra is a tubular structure that extends from the bladder to the external opening.
- Structure: The length of the urethra varies between sexes. In females, the urethra is short (about 4 cm) and exits just above the vaginal opening. In males, the urethra is longer (about 20 cm) and passes through the prostate gland and penis.
- Function: The urethra transports urine from the bladder to the outside of the body during urination. In males, it also serves as a passage for semen during ejaculation.
Function of the Urinary System
The urinary system has several key functions that are vital to maintaining the body’s internal balance:
- Filtration: The kidneys filter blood, removing metabolic waste products such as urea, creatinine, and uric acid. This process occurs in the glomeruli, where blood pressure forces fluid and small molecules through the filtration membrane, producing a filtrate that is processed to form urine.
- Reabsorption: Essential substances such as glucose, amino acids, ions, and water are reabsorbed from the filtrate back into the blood in the proximal convoluted tubules and loop of Henle.
- Secretion: The kidneys actively secrete additional waste products, ions, and drugs from the blood into the filtrate, particularly in the distal convoluted tubules and collecting ducts.
- Excretion: The final urine, composed of water, electrolytes, and waste products, is excreted from the body through the ureters, bladder, and urethra.
- Regulation of Blood Pressure: The kidneys regulate blood pressure through the renin-angiotensin-aldosterone system (RAAS). Renin, released by the kidneys, leads to the production of angiotensin II, which constricts blood vessels and stimulates aldosterone secretion to increase blood volume and pressure.
- Electrolyte and pH Balance: The kidneys maintain the balance of key electrolytes (such as sodium, potassium, and calcium) and regulate blood pH by excreting hydrogen ions and reabsorbing bicarbonate ions.
- Hormone Production: The kidneys produce the hormone erythropoietin, which stimulates red blood cell production in the bone marrow in response to low oxygen levels. They also activate vitamin D, which is essential for calcium absorption in the intestines.
Regulation of Kidney Function
Kidney function is regulated by several hormonal and neural mechanisms:
- Antidiuretic Hormone (ADH): Secreted by the posterior pituitary gland, ADH increases water reabsorption in the collecting ducts, concentrating urine and conserving water.
- Aldosterone: Produced by the adrenal glands, aldosterone promotes sodium reabsorption and potassium excretion in the distal convoluted tubule, increasing blood volume and pressure.
- Atrial Natriuretic Peptide (ANP): Released by the heart in response to high blood pressure, ANP reduces sodium reabsorption, promoting the excretion of sodium and water to lower blood pressure.
Clinical Relevance
Disorders of the urinary system can affect kidney function, fluid balance, and waste elimination, leading to a wide range of clinical conditions:
- Chronic Kidney Disease (CKD): A long-term, progressive loss of kidney function that can lead to kidney failure (end-stage renal disease) if untreated. Common causes include diabetes and hypertension. CKD is diagnosed through blood tests (measuring creatinine and glomerular filtration rate) and urinalysis.
- Urinary Tract Infections (UTIs): Bacterial infections that can affect any part of the urinary system, most commonly the bladder and urethra. Symptoms include painful urination, frequent urination, and cloudy or foul-smelling urine. UTIs are more common in females due to the shorter urethra.
- Kidney Stones (Nephrolithiasis): Hard deposits of minerals (such as calcium oxalate) that form in the kidneys and can obstruct urine flow. Kidney stones cause severe pain, especially during passage through the ureters. Treatment may involve pain management, hydration, or lithotripsy (breaking up the stones with sound waves).
- Acute Kidney Injury (AKI): A sudden decline in kidney function due to trauma, dehydration, infection, or nephrotoxic drugs. AKI can lead to electrolyte imbalances, fluid retention, and the accumulation of waste products in the blood.
- Glomerulonephritis: Inflammation of the glomeruli, often caused by immune system dysfunction, infections, or chronic diseases such as lupus. It can result in proteinuria, hematuria (blood in the urine), and decreased kidney function.
- Polycystic Kidney Disease (PKD): A genetic disorder characterized by the growth of numerous cysts in the kidneys, which can lead to kidney failure over time.
- Urinary Incontinence: The inability to control urination, often caused by weakened pelvic floor muscles, nerve damage, or an overactive bladder. Treatments may include pelvic floor exercises, medications, or surgery.
- Benign Prostatic Hyperplasia (BPH): An enlargement of the prostate gland in men, which can compress the urethra and cause difficulty urinating. Treatment options include medications or surgery to reduce prostate size.
Diagnostic and Therapeutic Approaches
Several diagnostic tools and treatments are available for managing urinary system disorders:
- Urinalysis: A routine test that analyzes the content of urine, detecting the presence of proteins, blood, glucose, bacteria, or abnormal cells, which can indicate infection or kidney dysfunction.
- Blood Tests: Serum creatinine and blood urea nitrogen (BUN) levels are measured to assess kidney function. Elevated levels indicate impaired kidney function or the presence of kidney disease. Glomerular filtration rate (GFR) is also calculated to estimate how efficiently the kidneys are filtering blood.
- Imaging Studies:
- Ultrasound: Non-invasive imaging used to visualize the kidneys, ureters, and bladder, and to detect kidney stones, cysts, or blockages.
- CT Scan: Provides detailed images to diagnose kidney stones, tumors, or abnormalities in the urinary tract.
- Intravenous Pyelogram (IVP): Involves injecting a contrast dye into the bloodstream to take X-rays of the kidneys and urinary tract, helping diagnose structural abnormalities or obstructions.
- Biopsy: In cases where kidney disease is suspected, a small sample of kidney tissue may be taken for examination under a microscope. This can provide information about the cause and severity of kidney damage.
- Cystoscopy: A procedure in which a thin, flexible tube with a camera (cystoscope) is inserted through the urethra to examine the inside of the bladder and urethra. It is commonly used to diagnose bladder issues, such as tumors, stones, or infections.
- Dialysis: A life-saving treatment for patients with advanced kidney failure (end-stage renal disease), dialysis helps remove waste products and excess fluid from the blood. There are two main types of dialysis:
- Hemodialysis: Blood is filtered through a machine outside the body and returned to the bloodstream.
- Peritoneal Dialysis: A dialysis solution is introduced into the peritoneal cavity, and waste products diffuse into the solution, which is later drained.
- Kidney Transplant: For patients with end-stage renal disease, a kidney transplant may be the best treatment option. It involves replacing the failed kidney with a healthy donor kidney.
- Medications: Various drugs are used to manage urinary system disorders:
- Diuretics: Help increase urine output and reduce fluid buildup in cases of hypertension, heart failure, or kidney disease.
- Antibiotics: Used to treat urinary tract infections.
- ACE inhibitors and ARBs: Used to protect kidney function in patients with diabetes or hypertension.
Conclusion
The urinary system is essential for maintaining fluid and electrolyte balance, filtering waste products from the blood, and regulating blood pressure. Understanding the structure and function of the kidneys, ureters, bladder, and urethra is crucial for diagnosing and managing disorders that can impact this system. Advances in diagnostic tools, medications, and treatments such as dialysis and kidney transplantation have improved the management of kidney diseases and enhanced the quality of life for patients with urinary system disorders.
References
- Standring, S. (2020). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (42nd ed.). Elsevier.
- Moore, K. L., Dalley, A. F., & Agur, A. M. R. (2013). Clinically Oriented Anatomy (7th ed.). Lippincott Williams & Wilkins.
- National Kidney Foundation. Chronic Kidney Disease (CKD) Guidelines.
- Brenner, B. M., & Rector, F. C. (2012). The Kidney (9th ed.). Elsevier.
- Levey, A. S., & Coresh, J. (2012). Chronic kidney disease. The Lancet, 379(9811), 165-180.
This detailed exploration of the urinary system highlights its vital role in maintaining homeostasis and emphasizes the importance of early diagnosis and treatment of kidney-related conditions.
🎓 Want to become a certified instructor?
This lesson is part of our FREE Anatomy course. Create a free account to track your progress and earn your certificate!