The Veins of the Body: Structure, Function, and Clinical Relevance
Abstract
The veins are an essential component of the circulatory system, responsible for returning deoxygenated blood from the tissues back to the heart. Veins operate under lower pressure than arteries and have specialized structures to prevent the backflow of blood. This article provides an expansive overview of the anatomy, function, and clinical relevance of the venous system.
Introduction
The venous system plays a critical role in maintaining circulation by transporting deoxygenated blood from tissues back to the heart and lungs for oxygenation. Veins are less muscular than arteries but are equipped with valves to facilitate blood flow against gravity, especially in the lower extremities. Understanding the anatomy and function of the veins is crucial in fields such as cardiology, vascular surgery, and internal medicine.
Structure of Veins
Similar to arteries, veins consist of three layers, though these layers are thinner due to the lower pressure within the venous system:
- Tunica Intima (Inner Layer): A smooth endothelial lining that reduces friction for blood flow and contains valves in many veins, especially in the limbs, to prevent blood backflow.
- Tunica Media (Middle Layer): Composed of smooth muscle, it is much thinner in veins compared to arteries, allowing for greater flexibility but less contraction.
- Tunica Externa (Outer Layer): Made up of connective tissue, this layer provides structural support and protects the veins.
Types of Veins
Veins are classified into three major types based on their size and function:
- Superficial Veins: Located close to the surface of the skin, these veins are often visible and do not run alongside major arteries.
- Deep Veins: Located deeper within the body, these veins run parallel to arteries and are responsible for draining the majority of blood from the limbs.
- Perforating Veins: These veins connect superficial veins to deep veins, allowing for the transfer of blood between the two systems.
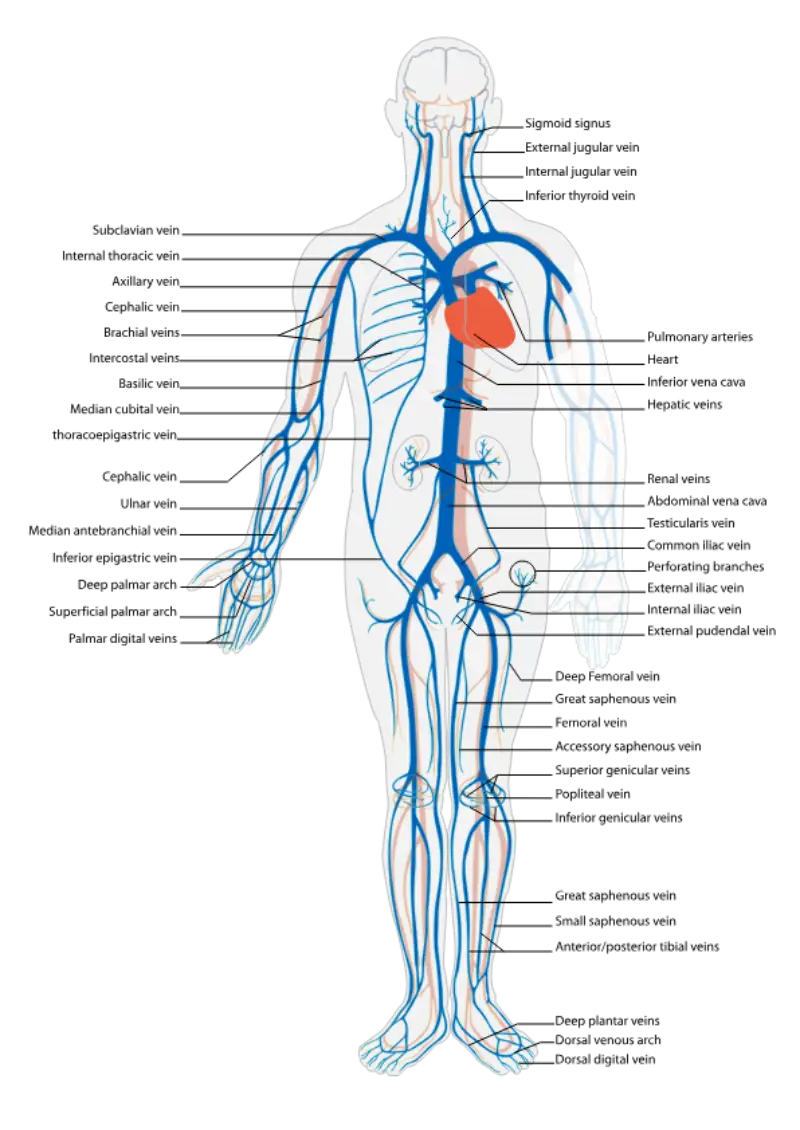
Major Veins of the Body
The venous system can be divided into several regions, each responsible for draining specific areas of the body.
Veins of the Head and Neck
- Jugular Veins:
- Internal Jugular Vein: Drains blood from the brain, face, and neck, emptying into the brachiocephalic vein.
- External Jugular Vein: Drains blood from the superficial regions of the face, scalp, and neck.
- Vertebral Veins: Accompany the vertebral arteries and drain the cervical vertebrae, spinal cord, and muscles of the neck.
- Dural Venous Sinuses: These large, endothelium-lined venous channels within the dura mater of the brain drain blood from the brain into the internal jugular veins.
Veins of the Upper Limb
- Subclavian Vein: Continuation of the axillary vein, draining blood from the upper limb into the brachiocephalic vein.
- Axillary Vein: Formed by the convergence of the brachial and basilic veins, it drains blood from the upper arm and shoulder.
- Brachial Vein: Runs alongside the brachial artery, draining blood from the deep structures of the arm.
- Cephalic Vein: A superficial vein that runs along the lateral side of the arm and empties into the axillary vein.
- Basilic Vein: A superficial vein that runs along the medial side of the arm and empties into the brachial vein.
- Median Cubital Vein: A superficial vein that connects the basilic and cephalic veins at the elbow, commonly used for venipuncture.
Veins of the Thorax
- Superior Vena Cava: Formed by the union of the brachiocephalic veins, the superior vena cava drains deoxygenated blood from the upper half of the body into the right atrium of the heart.
- Azygos Vein: Drains blood from the thoracic wall and posterior intercostal veins, eventually emptying into the superior vena cava.
- Hemiazygos and Accessory Hemiazygos Veins: Serve as counterparts to the azygos vein, draining blood from the lower thoracic and lumbar regions on the left side.
Veins of the Abdomen
- Inferior Vena Cava: The largest vein in the body, the inferior vena cava drains deoxygenated blood from the lower half of the body into the right atrium of the heart. It is formed by the convergence of the common iliac veins.
- Hepatic Veins: Drain blood from the liver into the inferior vena cava.
- Renal Veins: Drain blood from the kidneys into the inferior vena cava.
- Gonadal Veins: Drain blood from the testes in males and ovaries in females.
- The right gonadal vein empties into the inferior vena cava, while the left gonadal vein drains into the left renal vein.
- Lumbar Veins: Drain blood from the lumbar spine and posterior abdominal wall into the inferior vena cava.
Veins of the Pelvis and Lower Limb
- Common Iliac Veins: Formed by the union of the internal and external iliac veins, these veins drain blood from the pelvis and lower limbs into the inferior vena cava.
- Internal Iliac Veins: Drain blood from the pelvic organs, including the bladder, rectum, and reproductive organs.
- External Iliac Veins: Continue from the femoral veins and drain blood from the lower limbs.
- Femoral Veins: Drain blood from the thigh and receive blood from the deep femoral vein.
- Great Saphenous Vein: The longest vein in the body, running superficially from the foot to the groin, it empties into the femoral vein. It is commonly used in coronary artery bypass graft (CABG) surgery.
- Small Saphenous Vein: A superficial vein that runs along the posterior aspect of the leg and empties into the popliteal vein.
- Popliteal Vein: Drains blood from the knee and lower leg, continuing as the femoral vein.
- Anterior and Posterior Tibial Veins: Drain blood from the anterior and posterior compartments of the lower leg, respectively.
Veins of the Hepatic Portal System
The hepatic portal system is a unique venous system that carries blood from the gastrointestinal tract to the liver for detoxification and processing before it enters the systemic circulation.
- Hepatic Portal Vein: Formed by the union of the superior mesenteric and splenic veins, it transports nutrient-rich blood from the gastrointestinal organs to the liver.
- Superior Mesenteric Vein: Drains blood from the small intestine, large intestine, and stomach.
- Inferior Mesenteric Vein: Drains blood from the distal part of the large intestine.
- Splenic Vein: Drains blood from the spleen, pancreas, and parts of the stomach.
Function of Veins
The primary function of veins is to return deoxygenated blood from the tissues back to the heart. This is achieved through several mechanisms:
- Low-Pressure System: Veins operate under much lower pressure than arteries, which is why they rely on other mechanisms to ensure the return of blood to the heart.
- Valves: Many veins, especially in the limbs, are equipped with one-way valves that prevent the backflow of blood and facilitate venous return against gravity.
- Muscle Pump: Contraction of skeletal muscles during movement compresses veins, pushing blood toward the heart.
- Respiratory Pump: Changes in pressure within the thoracic cavity during breathing also aid in the return of venous blood to the heart.
Clinical Relevance
Disorders affecting the veins can lead to significant clinical problems, often compromising the return of blood to the heart and leading to complications.
- Varicose Veins: A condition where superficial veins, particularly in the lower extremities, become enlarged and twisted due to valve failure, leading to blood pooling and increased pressure in the veins.
- Deep Vein Thrombosis (DVT): A serious condition where blood clots form in the deep veins, usually in the legs. If left untreated, these clots can travel to the lungs, causing a life-threatening pulmonary embolism.
- Chronic Venous Insufficiency (CVI): A condition where the veins in the legs fail to efficiently return blood to the heart, leading to swelling, skin changes, and ulcers.
- Pulmonary Embolism: A condition where a blood clot from the deep veins of the legs (DVT) travels to the lungs, causing a blockage in the pulmonary arteries, which can be life-threatening.
- Portal Hypertension: Increased pressure in the portal venous system, usually due to liver cirrhosis, can lead to complications such as esophageal varices, ascites, and hepatic encephalopathy.
- Superior Vena Cava Syndrome: Compression or obstruction of the superior vena cava, often due to tumors or thrombosis, leading to swelling of the face, neck, and upper limbs, as well as difficulty breathing.
Diagnostic and Therapeutic Approaches
Diagnosis of venous disorders typically involves clinical examination, imaging techniques, and functional tests to assess blood flow.
- **Doppler
Ultrasound**: A non-invasive imaging technique used to assess blood flow through veins and detect the presence of blood clots or venous insufficiency. 2. Venography: An imaging test that involves injecting contrast dye into a vein to visualize the venous system, particularly in cases of suspected deep vein thrombosis. 3. Blood Tests: D-dimer testing is often used to detect the presence of blood clots in conditions like deep vein thrombosis or pulmonary embolism. 4. Compression Therapy: The use of compression stockings is a common non-invasive treatment for varicose veins and chronic venous insufficiency. 5. Anticoagulation Therapy: Medications like heparin and warfarin are commonly used to treat conditions such as DVT and pulmonary embolism by preventing clot formation and extension. 6. Sclerotherapy and Ablation: Procedures used to treat varicose veins by closing off the affected veins and rerouting blood flow to healthier veins. 7. Surgical Interventions: In severe cases of venous disease, surgery may be necessary, such as in the treatment of varicose veins or for removing large clots in cases of DVT.
Conclusion
The veins of the body are critical for the return of deoxygenated blood to the heart and the removal of metabolic waste from tissues. Understanding the structure, function, and disorders associated with the venous system is essential for managing venous diseases and maintaining circulatory health. Advances in diagnostic techniques and treatment options continue to improve the management of venous conditions, enhancing patient outcomes and quality of life.
References
- Standring, S. (2020). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (42nd ed.). Elsevier.
- Moore, K. L., Dalley, A. F., & Agur, A. M. R. (2013). Clinically Oriented Anatomy (7th ed.). Lippincott Williams & Wilkins.
- Netter, F. H. (2014). Atlas of Human Anatomy (6th ed.). Elsevier.
- Williams, P. L., & Warwick, R. (1980). Gray’s Anatomy (36th ed.). Churchill Livingstone.
- Khan, S. R., & Zia, E. (2021). Deep Vein Thrombosis. In StatPearls. StatPearls Publishing.
- Meissner, M. H., Gloviczki, P., & Bergan, J. J. (2009). Chronic Venous Insufficiency and Varicose Veins. Journal of Vascular Surgery, 49(3), 734-739.
This comprehensive exploration of the veins of the body emphasizes their crucial role in the circulatory system, while highlighting the importance of research and education in managing venous diseases.
🎓 Want to become a certified instructor?
This lesson is part of our FREE Anatomy course. Create a free account to track your progress and earn your certificate!