The Human Pelvis: Structure, Function, and Clinical Relevance
Abstract
The human pelvis is a complex, bony structure that forms the base of the spine and the socket for the femur in each leg. It plays critical roles in supporting the weight of the upper body, enabling locomotion, and housing and protecting the pelvic organs. This article explores the detailed anatomy, development, functions, and clinical significance of the human pelvis.
Introduction
The pelvis, often referred to as the pelvic girdle, is an essential structure in the human skeleton. It connects the spine to the lower limbs, supports the body’s weight during sitting and standing, and protects the pelvic and abdominal organs. Understanding the pelvis’s anatomy and function is vital for fields such as orthopedics, gynecology, urology, and physical therapy.
Anatomical Structure
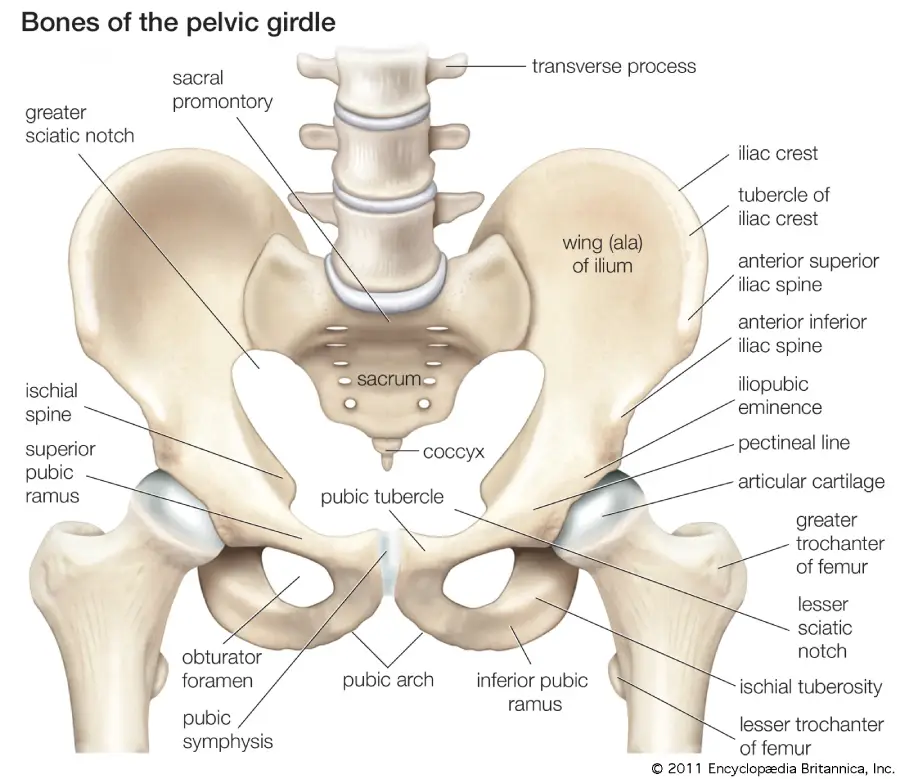
The pelvis is composed of several bones that fuse together in adulthood:
- Hip Bones (Ilium, Ischium, Pubis)
- Sacrum
- Coccyx
Each hip bone (os coxae) is formed by the fusion of three bones:
- Ilium: The broad, flaring portion.
- Ischium: The lower, posterior part.
- Pubis: The anterior portion.
Ilium
The ilium is the largest part of the hip bone, contributing to the superior region of the pelvis. Key features include:
- Iliac Crest: The superior border, serving as an attachment for muscles.
- Anterior Superior Iliac Spine (ASIS): A landmark for various anatomical and clinical purposes.
- Iliac Fossa: The concave surface that supports abdominal organs.
Ischium
The ischium forms the lower and back part of the hip bone. Notable parts include:
- Ischial Tuberosity: The part we sit on, providing attachment for the hamstring muscles.
- Ischial Spine: A point of attachment for ligaments and muscles.
Pubis
The pubis is the anterior part of the hip bone. Important structures include:
- Pubic Symphysis: A cartilaginous joint uniting the left and right pubic bones.
- Superior and Inferior Pubic Rami: Extensions that connect to the ilium and ischium, respectively.
Sacrum and Coccyx
- Sacrum: A triangular bone formed by the fusion of five sacral vertebrae, connecting the spine to the pelvis.
- Coccyx: Commonly known as the tailbone, formed by the fusion of four coccygeal vertebrae.
Pelvic Joints and Ligaments
The pelvis is stabilized by several joints and ligaments:
- Sacroiliac Joints: Connect the sacrum to the ilium.
- Pubic Symphysis: Joins the two pubic bones.
- Sacrospinous and Sacrotuberous Ligaments: Provide additional stability by connecting the sacrum to the ischium.
Development
The pelvis develops through endochondral ossification:
- Primary Ossification Centers: Appear in the ilium, ischium, and pubis during fetal development.
- Secondary Ossification Centers: Develop during adolescence, contributing to the growth and final shape of the pelvis.
- Fusion: The ilium, ischium, and pubis fuse in late adolescence to form the mature hip bone.
Function
The pelvis serves several vital functions:
- Support: Bears the weight of the upper body and transfers it to the lower limbs.
- Protection: Shields pelvic and abdominal organs, including the bladder, rectum, and reproductive organs.
- Movement: Provides attachment points for muscles involved in locomotion and posture.
- Childbirth: In females, the pelvis is adapted to facilitate the passage of the newborn during delivery.
Sex Differences in the Pelvis
Male and female pelves exhibit distinct differences due to reproductive functions:
- Female Pelvis: Broader, shallower, with a wider pelvic inlet and outlet to accommodate childbirth.
- Male Pelvis: Narrower, deeper, with a more pronounced sacral promontory and ischial spines.
Clinical Relevance
The pelvis is involved in various medical conditions and injuries:
- Fractures: Can result from trauma and may affect the stability and function of the pelvic ring.
- Osteoarthritis: Degeneration of the hip joint can lead to pain and reduced mobility.
- Pelvic Inflammatory Disease (PID): Infections of the female reproductive organs can cause pelvic pain and infertility.
- Pelvic Floor Disorders: Include conditions like prolapse and incontinence, often resulting from weakened pelvic muscles.
- Hip Dysplasia: A developmental disorder where the hip socket is shallow, leading to instability and potential dislocation.
Diagnostic and Therapeutic Approaches
Diagnosis of pelvic disorders typically involves imaging techniques such as X-rays, MRI, and CT scans. Treatment options vary depending on the condition and may include:
- Physical Therapy: Exercises to strengthen pelvic muscles and improve function.
- Medications: Pain relievers, anti-inflammatory drugs, and antibiotics for infections.
- Surgical Interventions: Procedures like hip replacement, pelvic fracture repair, and corrective surgery for pelvic floor disorders.
Conclusion
The human pelvis is a crucial structure that supports and stabilizes the body, protects vital organs, and plays a key role in locomotion and reproduction. Understanding its anatomy, development, and associated pathologies is essential for effective medical care. Advances in diagnostic imaging and surgical techniques continue to improve the management of pelvic disorders, enhancing patient outcomes.
References
- Standring, S. (2020). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (42nd ed.). Elsevier.
- Moore, K. L., Dalley, A. F., & Agur, A. M. R. (2013). Clinically Oriented Anatomy (7th ed.). Lippincott Williams & Wilkins.
- Sadler, T. W. (2018). Langman’s Medical Embryology (14th ed.). Wolters Kluwer.
- Goss, C. M. (2010). Anatomy of the Human Body. Lea & Febiger.
- Nordin, M., & Frankel, V. H. (2001). Basic Biomechanics of the Musculoskeletal System (3rd ed.). Lippincott Williams & Wilkins.
This detailed examination of the human pelvis highlights its complexity and importance, emphasizing the need for continued research and education in pelvic health and disease management.
🎓 Want to become a certified instructor?
This lesson is part of our FREE Anatomy course. Create a free account to track your progress and earn your certificate!