The Muscles of the Upper Extremity: Structure, Function, and Clinical Relevance
Medical disclaimer: Educational content only. For diagnosis and treatment, consult a licensed clinician.
Abstract
The muscles of the upper extremity (shoulder, arm, forearm, and hand) enable both power and precision. This article integrates anatomy, biomechanics, injury mechanisms, diagnostic pathways (MRI, ultrasound, EMG), and evidence-based rehabilitation. Clinically rich sections target common conditions such as rotator cuff tears, carpal tunnel syndrome, lateral epicondylitis, and ulnar neuropathy, alongside ergonomic and occupational health considerations.
Introduction
Modern work patterns such as prolonged keyboard use, device overuse, and manual handling elevate risk for overuse injuries and nerve compression syndromes. Understanding upper limb anatomy helps clinicians, therapists, coaches, and students design rehabilitation and prevention strategies grounded in orthopedics, physical therapy, sports medicine, and occupational health.
📋 Table of Contents
Jump to any section:
-
Anatomical Structure - Overview of the 4 major muscle groups
- Muscles of the Shoulder - Rotator cuff and scapular stabilizers
- Muscles of the Arm - Elbow flexors and extensors
- Muscles of the Forearm - Wrist and finger control
- Muscles of the Hand - Intrinsic muscles for dexterity
-
Development - Embryologic origins (somites to myotomes)
-
Function - Movement, stabilization, force, fine motor control
-
Clinical Relevance - High-impact conditions and differentials
-
Diagnostics and Treatment - Imaging, EMG, conservative care, injections, surgery
-
Rehabilitation and Ergonomics - Protocols, return to work, prevention
-
FAQs - Cost, braces, recovery time, home vs clinic therapy
-
Conclusion - Key takeaways
Anatomical Structure
Upper extremity muscles are grouped by region:
- Shoulder (Scapular and Thoracic)
- Arm (Brachium)
- Forearm (Antebrachium)
- Hand (Intrinsic and Extrinsic)
Muscles of the Shoulder
Primary roles: glenohumeral stability, range of motion, force coupling.
Extrinsic Shoulder Muscles
- Trapezius: Scapular elevation and retraction; assists cervical extension.
- Latissimus dorsi: Shoulder extension, adduction, internal rotation.
- Levator scapulae: Scapular elevation and cervical rotation.
- Rhomboids: Scapular retraction and downward rotation.
Intrinsic Shoulder Muscles
 Figure: Muscles that Position the Pectoral Girdle - Anterior View (OpenStax, CC BY 4.0)
Figure: Muscles that Position the Pectoral Girdle - Anterior View (OpenStax, CC BY 4.0)
- Deltoid: Abduction; anterior and posterior fibers flex and extend.
- Teres major: Extension, adduction, internal rotation.
- Rotator cuff: Supraspinatus (abduction), Infraspinatus (external rotation), Teres minor (external rotation and adduction), Subscapularis (internal rotation).
Figure: The Rotator Cuff (CC BY-SA 4.0)
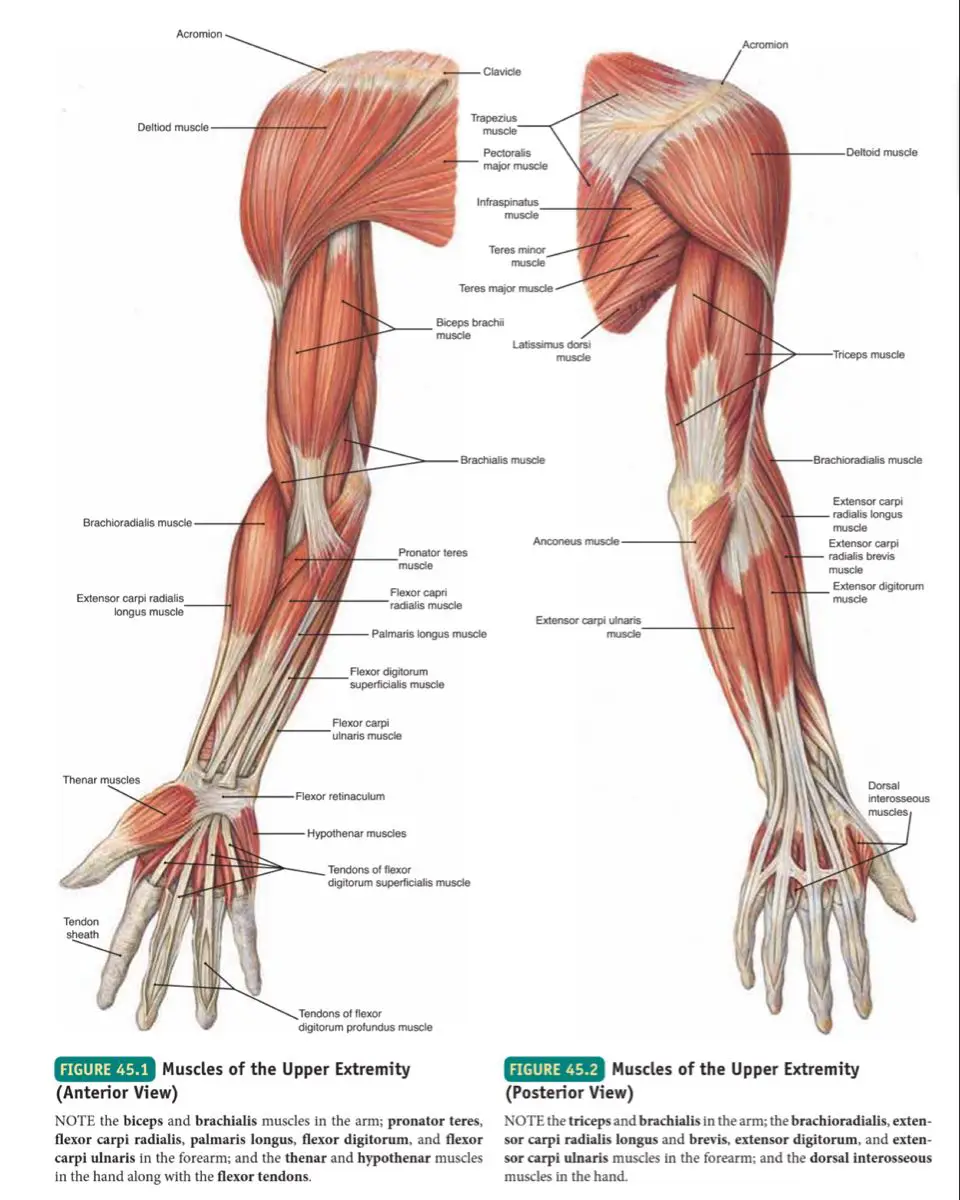
Muscles of the Arm
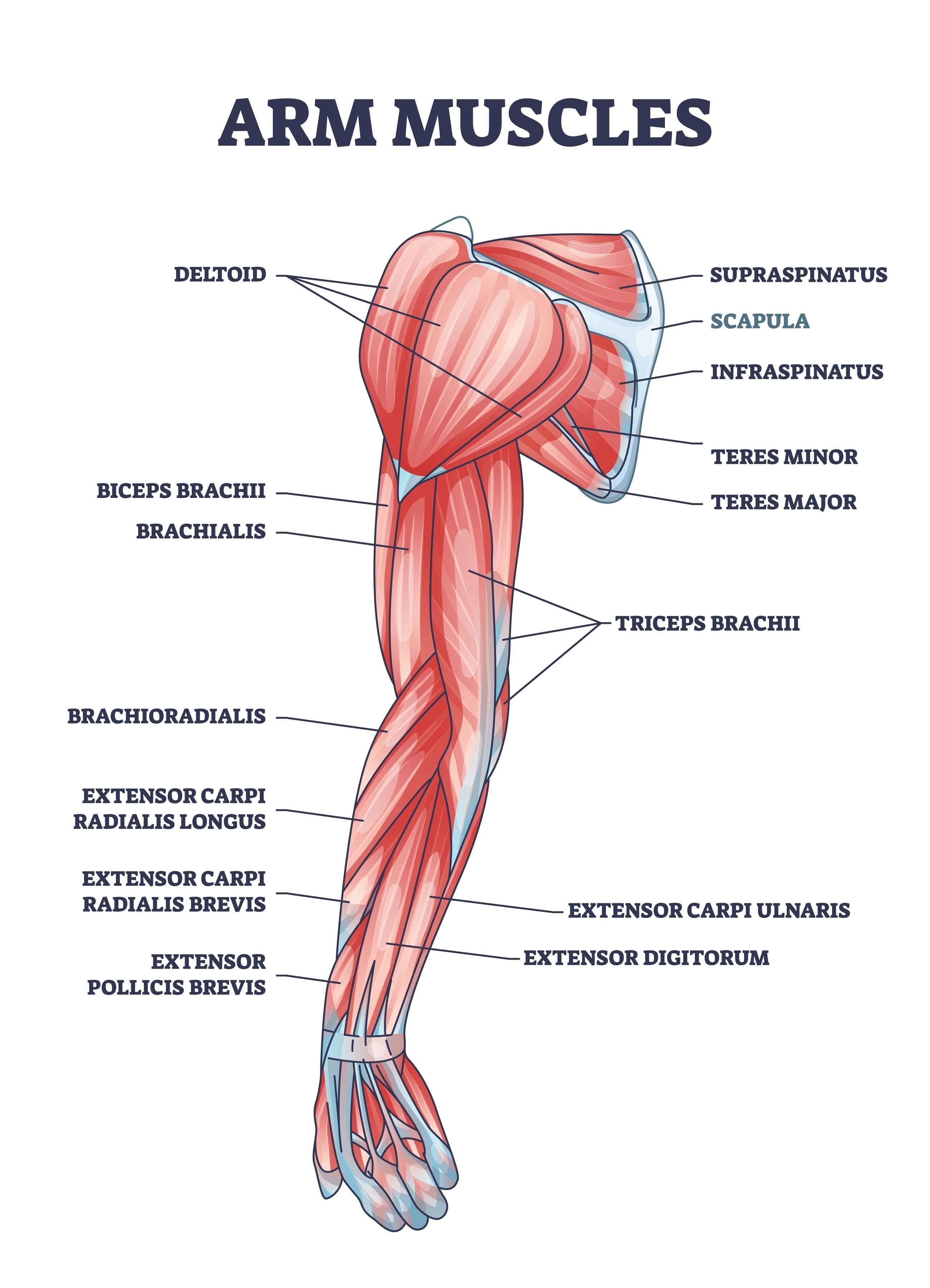
Anterior: Biceps brachii (elbow flexion and supination), Brachialis (primary elbow flexor), Coracobrachialis (shoulder flexion and adduction).
Posterior: Triceps brachii (elbow extension), Anconeus (terminal extension and stability).
Muscles of the Forearm
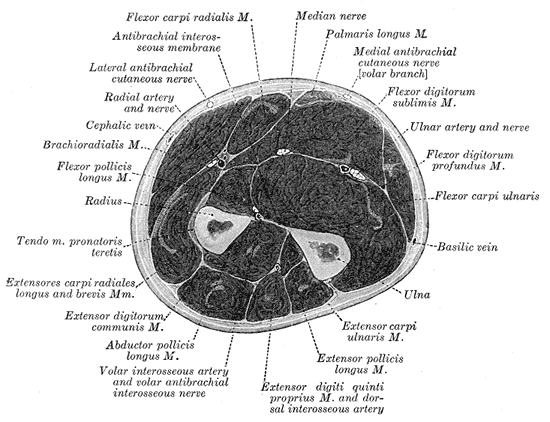 Figure: Anterior Forearm - Flexors (Gray’s Anatomy, Public Domain)
Figure: Anterior Forearm - Flexors (Gray’s Anatomy, Public Domain)
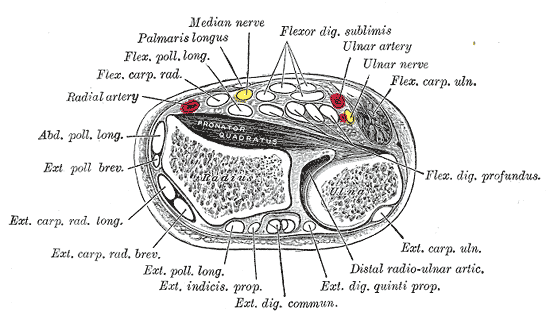 Figure: Posterior Forearm - Extensors (Gray’s Anatomy, Public Domain)
Figure: Posterior Forearm - Extensors (Gray’s Anatomy, Public Domain)
Anterior (flexors and pronators)
- Superficial: Pronator teres, FCR, Palmaris longus, FCU
- Intermediate: FDS
- Deep: FDP, FPL, Pronator quadratus
Posterior (extensors and supinators)
- Superficial: Brachioradialis, ECRL, ECRB, Extensor digitorum, EDM, ECU
- Deep: Supinator, APL, EPL and EPB, Extensor indicis
Muscles of the Hand
 Figure: Intrinsic Hand Muscles (OpenStax, CC BY 4.0)
Figure: Intrinsic Hand Muscles (OpenStax, CC BY 4.0)
Intrinsic: Thenar (APB, FPB, OP), Hypothenar (ADM, FDM, ODM), Lumbricals, Interossei (dorsal abduct and palmar adduct), Adductor pollicis.
Extrinsic: FDS, FDP, FPL, Extensor digitorum, EPL and EPB.
Development
Upper limb musculature derives from paraxial mesoderm (somites to myotomes).
- Epaxial leads to deep back muscles.
- Hypaxial leads to limb musculature (upper and lower extremities).
Function
- Movement: Flexion and extension, abduction and adduction, rotation, circumduction.
- Stabilization: Dynamic joint stability at shoulder, elbow, and wrist.
- Force generation: Lifting, pushing, pulling.
- Fine motor: Writing, instrument playing, precision grip.
- Grip and manipulation: Power and precision prehension.
The in-depth knowledge of movement and force required for advanced clinical practice is often the core focus of a specialized biomechanics class.
Clinical Relevance
High-impact conditions with frequent search interest and advertiser demand:
| Condition | Key Features | At-Risk Activities | First-Line Management |
|---|---|---|---|
| Rotator cuff tear or impingement | Painful arc, night pain, weakness | Overhead work, throwing | Physical therapy with scapular and rotator cuff strengthening, NSAIDs; consider MRI |
| Carpal tunnel syndrome | Nocturnal paresthesia, thenar weakness | Typing, assembly line | Neutral wrist splint, activity modification; ultrasound-guided corticosteroid injection or surgery |
| Tennis elbow (lateral epicondylitis) | Pain over lateral epicondyle | Repetitive wrist extension | Eccentric loading, counterforce strap; shockwave or PRP as needed |
| Cubital tunnel syndrome | Ulnar digit paresthesia | Elbow flexion posture | Night elbow splinting; surgical decompression if persistent |
| De Quervain’s tenosynovitis | Radial wrist pain; positive Finkelstein | Infant care, texting | Thumb spica splint, NSAIDs; steroid injection |
| Dupuytren’s contracture | Palmar nodules, finger flexion deformity | Genetic predisposition | Collagenase injection or fasciectomy |
When to seek care: Red-flag symptoms such as acute trauma, severe weakness, progressive numbness, deformity, or fever warrant prompt medical evaluation.
Diagnostics and Treatment
Imaging and Tests
- MRI shoulder or wrist for tendon tears and ligament injury.
- Ultrasound for dynamic tendon evaluation and guided injections.
- EMG and nerve conduction studies for median, ulnar, and radial neuropathies.
- X-ray for fractures and degeneration; grip dynamometry for function.
Conservative Therapy
- Physical Therapy: Scapular stabilization, rotator cuff strengthening, eccentric wrist extensors, nerve glides.
- Medications: NSAIDs and acetaminophen; short courses of corticosteroid injections when indicated.
- Manual Therapy: Joint mobilization, soft tissue techniques, taping.
- Ergonomic Adjustments: Keyboard and pointing device changes, forearm support, micro-breaks.
- Adjuncts: Shockwave therapy and PRP for tendinopathies (evidence varies).
- Surgery: Arthroscopic cuff repair, endoscopic or open carpal tunnel release, nerve decompression where conservative care fails.
Rehabilitation and Ergonomics
Sample evidence-informed protocol snippets (non-prescriptive):
-
Rotator cuff or impingement (6 to 12 weeks)
- Phase 1: Pain control, isometrics, scapular retraction and depression.
- Phase 2: External rotation with band, scaption, closed-chain stability.
- Phase 3: Sport or work conditioning and gradual overhead progressions.
-
Lateral epicondylitis (8 to 12 weeks)
- Eccentric wrist extension loading; forearm pronation and supination control.
- Counterforce strap during activity; progress to functional tasks.
-
Carpal tunnel
- Night neutral-wrist splinting; activity modification; tendon and nerve glides.
- Consider workplace ergonomic assessment and timed breaks.
Ergonomic quick wins
- Keyboard with low actuation force and split layout
- Vertical mouse or trackball to reduce forearm pronation
- Monitor at eye level; chair with lumbar support; elbows about 90 degrees
- 20-8-2 rule each half hour: 20 minutes sit, 8 minutes stand, 2 minutes movement
FAQs
How long does carpal tunnel recovery take?
Mild cases may improve in 6 to 12 weeks with splinting and ergonomics. Post-surgical recovery is commonly 2 to 6 weeks for light duties.
Do wrist braces and elbow straps help?
They can reduce load on symptomatic tissues during activity. Choose neutral wrist braces for CTS and counterforce straps for lateral epicondylitis. Always pair with therapeutic exercise.
Is MRI necessary for shoulder pain?
Not always. Start with clinical exam and physical therapy. MRI is considered when trauma, persistent weakness, or failed conservative care is present.
What is the role of PRP or shockwave?
These may be considered for chronic tendinopathies after structured rehab. Discuss risks, cost, and evidence with a clinician.
Conclusion
Upper extremity muscle health underpins human dexterity and quality of life. A combined approach that includes accurate diagnosis, progressive rehabilitation, and ergonomics optimizes outcomes and reduces recurrence. Ongoing advances in biomechanics and regenerative therapies continue to refine care pathways. Accurate documentation of upper extremity conditions is not only essential for clinical care but may also be a critical component in the event of a carpal tunnel lawsuit or other occupational health claim.
References
- Standring, S. Gray’s Anatomy: The Anatomical Basis of Clinical Practice (42nd ed.). Elsevier.
- Moore, K. L., Dalley, A. F., and Agur, A. M. R. Clinically Oriented Anatomy (7th ed.). LWW.
- Netter, F. H. Atlas of Human Anatomy (6th ed.). Elsevier.
- Williams, P. L., and Warwick, R. Gray’s Anatomy (36th ed.). Churchill Livingstone.
- Bogduk, N. Clinical Anatomy of the Lumbar Spine and Sacrum (4th ed.). Churchill Livingstone.
- Kendall, F. P., McCreary, E. K., and Provance, P. G. Muscles: Testing and Function, with Posture and Pain (5th ed.). LWW.
🎓 Want to become a certified instructor?
This lesson is part of our FREE Anatomy course. Create a free account to track your progress and earn your certificate!